How Trauma and Stress Contribute to Mental Health Conditions in Veterans
For many veterans, the transition from military service to civilian life is far more complex than it appears. Exposure to traumatic events and prolonged stress during deployment can leave lasting imprints on both the mind and body. These experiences don’t simply fade with time; they often contribute to the development of mental health conditions such as anxiety, depression, and post-traumatic stress disorder (PTSD). Understanding how trauma and stress impact veterans is essential in providing the right support, treatment, and compassion needed to help them rebuild their lives.
The Complex Nature of Military Trauma and Its Mental Health Impact
Think about this for a moment: military personnel encounter traumatic situations that most civilians will never experience. The psychological damage runs deeper than we often realize. What you’ll discover is that mental health conditions in veterans rarely stem from a single event. Instead, they emerge from layers of stress that build during service and persist long after discharge.
Combat-Related Trauma Triggers in Modern Warfare:
IED blasts don’t just wound, they rewire the brain. These explosive events create invisible injuries that compound every psychological scar. Your brain’s fear processing system gets permanently altered.
Losing battle buddies hits differently than civilian grief. The brotherhood forged in combat creates bonds unlike anything else. When those connections are severed by death, the surviving veterans carry wounds that civilian counselors often struggle to understand.
Then there’s moral injury, perhaps the most misunderstood form of trauma in veterans. Imagine being forced to act against your deepest values or witnessing unspeakable acts. This creates psychological damage that society barely acknowledges, let alone treats effectively.
Non-Combat Military Stressors Often Overlooked
Military sexual trauma affects service members of all genders. The betrayal cuts deep, violated by someone you’re supposed to trust with your life. Combine this with institutional challenges around reporting, and you have a recipe for complex, lasting trauma.
Toxic leadership and hazing create their own special hell. These experiences chip away at a person’s resilience, contributing to long-term military mental health issues that follow veterans home.
Multiple deployments tear families apart. The guilt of missing birthdays, anniversaries, and everyday moments while your family struggles at home? That weighs on veterans for years.
Given this broad spectrum of traumatic experiences, let’s examine how these varied stressors actually manifest as diagnosable conditions that veterans battle long after hanging up their uniforms.
Primary Mental Health Conditions Veterans Develop from Trauma Exposure
Here’s what the research tells us: veterans suffer disproportionately high rates of mental health conditions, including PTSD, depression, and substance abuse. These conditions often cluster together, creating treatment puzzles that require specialized expertise.
Post-Traumatic Stress Disorder (PTSD) Manifestations
Stress and PTSD create a vicious cycle where veterans become prisoners of their own memories. Flashbacks and nightmares transport them back to the worst moments of their service. A car backfiring or a helicopter overhead can trigger full-blown panic attacks.
Avoidance becomes a survival strategy. Veterans might dodge crowded malls, skip Fourth of July fireworks, or refuse to discuss their service entirely. They’re trying to outrun ghosts that live in their heads.
Hyperarousal keeps veterans trapped in combat mode. That constant vigilance served them well downrange, but it’s exhausting when you’re trying to grocery shop or attend your kid’s soccer game.
Depression and Anxiety Disorders in Military Personnel
Major depression often strikes hardest during the months following discharge. You lose your mission, your unit, your purpose, all at once. The structure that defined your existence vanishes overnight.
Generalized anxiety stems from a mind trained to spot threats everywhere. Veterans can’t simply flip a switch and turn off years of survival conditioning.
Social anxiety isolates veterans from civilian connections. How do you explain combat stress to someone whose biggest worry is their commute? The disconnect feels insurmountable.
Understanding these conditions matters, but what’s happening inside veterans’ brains during trauma exposure reveals why symptoms persist and points toward more effective treatments.
The Neurobiological Impact of Stress and PTSD on Veterans’ Brains
Here’s something fascinating: PTSD isn’t just psychological distress, it’s linked to altered metabolism. This connection explains why traditional talk therapy sometimes falls short of complete healing.
How Combat Stress Rewires Neural Pathways
The amygdala, your brain’s alarm system, gets stuck in overdrive among veterans with PTSD. It’s constantly scanning for danger, even during peaceful moments. Imagine your smoke detector going off every time you cook toast. Exhausting, right?
The hippocampus, crucial for memory formation, actually shrinks under chronic stress. Veterans may struggle creating new positive memories while traumatic ones remain crystal clear and intrusive.
Your prefrontal cortex, the rational thinking center, gets overwhelmed by the hyperactive fear response. This makes decision-making harder and emotional regulation nearly impossible.
Epigenetic Changes from Prolonged Military Stress
DNA methylation patterns change under severe stress. These alterations can be inherited by children, meaning military mental health challenges might echo through generations.
Gene expression shifts affect how your body handles future stressors. These changes can persist decades after the original trauma, explaining why some veterans struggle with symptoms that seem to come from nowhere.
Now that we understand how trauma literally rewires the brain, let’s explore the proven therapies and innovative treatments specifically designed to help veterans heal and reclaim their lives.
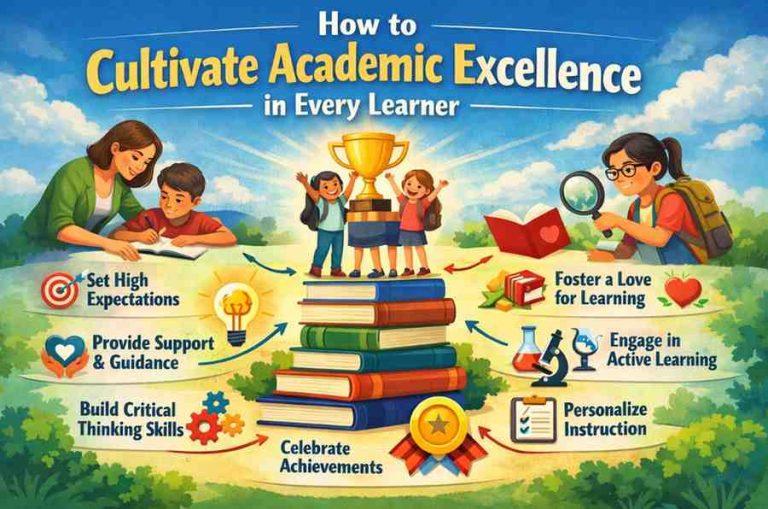
Evidence-Based Approaches for Coping with Trauma in Veterans
Good news: effective treatments exist, but they must respect military culture and experiences. Coping with trauma requires approaches that understand the unique context of military service.
Trauma-Focused Psychotherapy Methods
Cognitive Processing Therapy (CPT) tackles the guilt and self-blame that plague many veterans. It challenges those destructive thoughts that keep you stuck in trauma’s grip.
Prolonged Exposure therapy might sound scary, but it works by gradually reintroducing trauma memories in safe, controlled settings. Think of it as reclaiming your memories from trauma’s stranglehold.
Eye Movement Desensitization and Reprocessing (EMDR) processes traumatic memories through bilateral stimulation. Many veterans prefer this approach because it’s less emotionally draining than traditional talk therapy.
Building Resilience and Recovery Support Systems
Recovery happens in community, not isolation. Veterans need comprehensive support addressing every aspect of civilian transition.
Peer Support Networks That Transform Recovery
Veteran-to-veteran mentorship creates powerful healing connections. Who better to guide you through recovery than someone who’s walked your path?
Group therapy with fellow veterans breaks through isolation. Finally, you’re talking to people who truly get it, no explanations required.
Career Transition Support for Mental Health Stability
Skills translation helps veterans recognize how military experience transfers to civilian careers. This connection can restore purpose and identity.
Educational benefits open doors to new possibilities. Learning fresh skills often rebuilds confidence and self-worth that trauma damages.
Even with robust support systems and proven treatments available, many veterans still struggle accessing care due to persistent barriers that must be dismantled.
Breaking Down Barriers to Military Mental Health Treatment
Addressing Stigma and Cultural Resistance
Military culture still views seeking help as weakness. Leadership must actively promote the understanding that mental health conditions in veterans are treatable medical issues—not character flaws.
Cultural competency training helps civilian therapists understand military experiences. This knowledge improves treatment effectiveness and veteran comfort levels.
Navigating VA and Insurance Coverage Systems
Understanding VA disability ratings helps veterans access appropriate care. Many don’t realize they qualify for comprehensive mental health services.
Private insurance often provides faster access to treatment. Veterans shouldn’t have to choose between quality and speed of care.
Successfully removing treatment barriers is only half the equation, healing profoundly impacts loved ones who often experience their own trauma-related challenges requiring attention and support.
Family Impact and Secondary Trauma Considerations
Military families carry hidden costs of service alongside their veterans. Secondary trauma affects spouses, children, and parents witnessing their loved one’s struggles.
Supporting Military Spouses and Children
Children may develop behavioral issues when a parent returns changed by trauma. Family therapy helps everyone navigate these adjustments together.
Spouses often become untrained caregivers. They need their own resources to maintain mental health while supporting their veterans.
Community Integration and Social Reestablishment
Civilian employers benefit from education about veteran experiences. Understanding leads to better workplace accommodations and meaningful support.
Volunteer opportunities provide veterans renewed purpose. Contributing to communities helps rebuild identity beyond military service.
Given the complexity of veteran mental health and its ripple effects, specific questions naturally arise about symptoms, treatments, and practical concerns that deserve evidence-based answers.
Common Questions About Veteran Mental Health
What percentage of veterans experience mental health conditions after military service?
Research suggests approximately 20-30% of veterans face significant mental health challenges. Rates vary based on deployment history and combat exposure intensity.
How long after military service can PTSD symptoms first appear?
PTSD symptoms can emerge immediately or decades later. Delayed onset often occurs during major life transitions or additional stressors.
Can military trauma cause physical health problems beyond mental health issues?
Absolutely. Trauma manifests as chronic pain, sleep disorders, digestive problems, and cardiovascular issues. The mind-body connection runs deep.
Moving Forward: Hope for Healing
Healing from military trauma isn’t easy, but it’s absolutely achievable. Veterans deserve comprehensive support addressing both psychological and physical impacts of their service. By understanding how stress and PTSD affect the brain, implementing evidence-based treatments, and building strong support networks, we can help veterans reclaim their lives.
Remember this: seeking help isn’t weakness, it’s courage. It’s the next mission in a life of service. And just like every mission before, success is possible with the right support, tools, and determination.